
Products

GEM® Premier 7000 with iQM3
Preanalytical errors can impact point-of-care testing. What might you be missing?
Haemolysis, the #1 source of preanalytical error1, while prevalent throughout the hospital, is often unrecognised. This can negatively impact potassium (K+) results and patient care.2 For the first time integrated on a blood gas system, the GEM Premier 7000 with iQM3 detects and flags haemolysis, in just 45 seconds.11
A breakthrough in blood gas testing.

Haemolysis is the #1 source of preanalytical error¹
Preanalytical errors can affect the integrity of results in blood samples tested at the point of care (POC). Haemolysis accounts for up to 70% of all preanalytical errors and, while prevalent throughout the hospital, is often unrecognised. This can negatively impact potassium (K+) results and patient care.2
In vitro haemolysis can lead to:
- Inappropriate patient management3,6,7
- Decreased patient satisfaction6,8
- Inefficient staff/nursing time5,7,8
- Increased costs5,6,8
Haemolysis is prevalent throughout the hospital, and often unrecognised
Percentages indicate proportion of samples that are haemolysed in each clinical setting
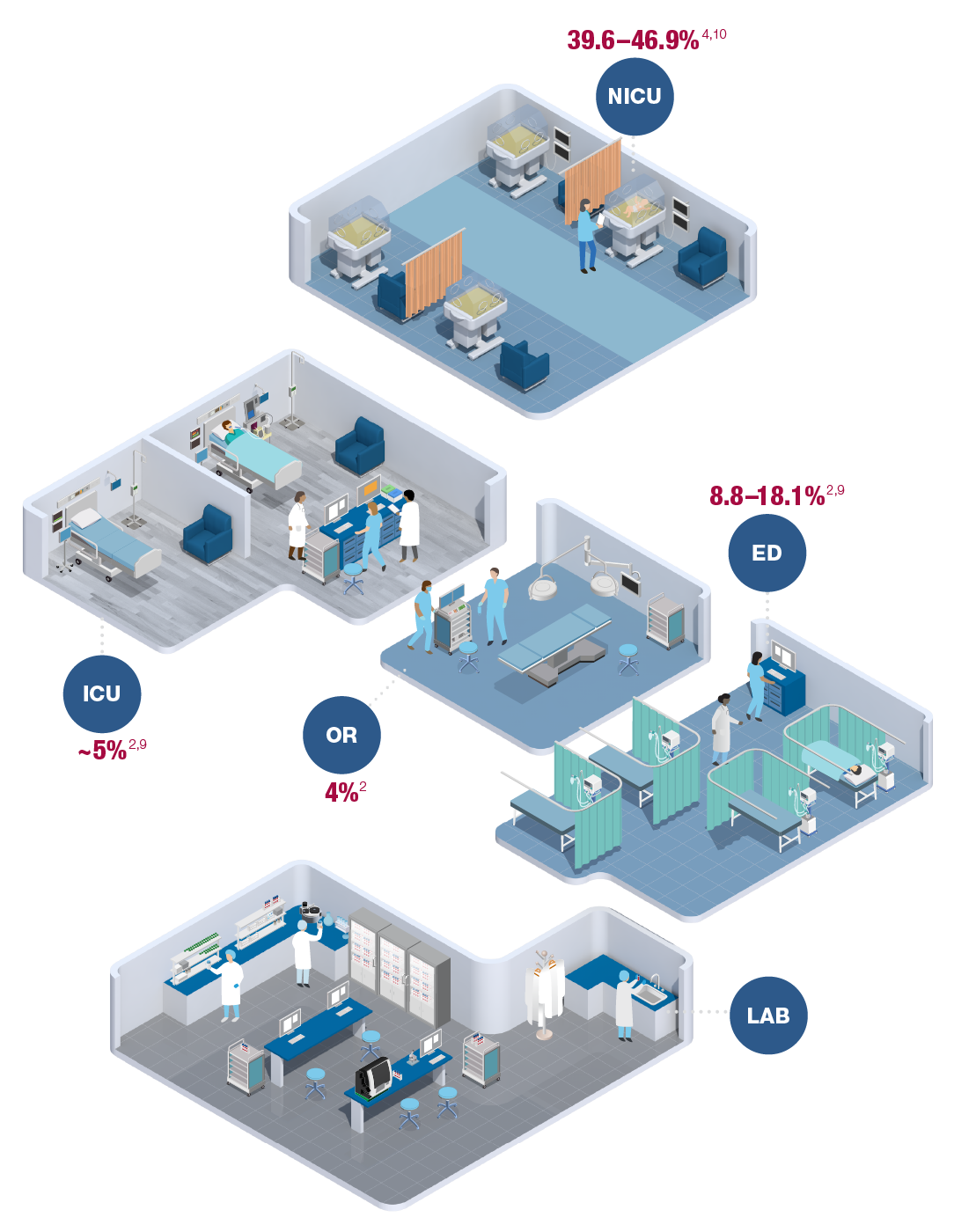
ICU-Intensive Care Unit; NICU–Neonatal Intensive Care Unit; OR–Operating Room; ED-Emergency Department
- iQM3 ensures sample quality across the most common preanalytical errors, detects haemolysis in 45 seconds11
- All-in-one GEM PAK cartridge automates labour- and skill-intensive processes
- GEMweb® Plus 500 Custom Connectivity simplifies control and compliance, enabling continuous quality improvement
GEM PAK: advanced simplicity at the POC
- Automates the most labour- and skill-intensive processes for improved productivity and cost-efficiency
- Self-contained and multi-use, limiting operator biohazard and infection exposure
- Room-temperature storage; no refrigeration required
- Replaced every 31 days—only 12 GEM PAKs/year/analyser**
- No hands-on troubleshooting or corrective actions required
- Variety of menu and test-volume configurations

Menu and PAK configurations
FLEXIBLE GEM PAK CUSTOMIZATION
Measured Analytes
pH, pCO2, pO2, Na+, K+, Cl–, Ca++, Glu, Lac, Hct, tBili, tHb, O2Hb, COHb, MetHb, HHb, sO2‡Derived (Calculated) Parameters
BE(B), BE(ecf), tHb(c), Ca++ (7.4), Anion gap (AG), P/F ratio, pAO2, CaO2, CvO2, p50, O2cap, sO2(c), O2ct, HCO3 – std, TCO2, HCO3 – (actual), A-aDO2, paO2/pAO2, RI, CcO2, a-vDO2, Qsp/Qt (est), Qsp/Qt, Hct(c), OI, OsmTest volumes
75, 100, 150, 300, 450, 600**
Menu options:
Blood Gas, Hct, tHb, O2Hb, HHb, COHb, MetHb, sO2, tBili***
Blood Gas, Electrolytes, Hct, tHb, O2Hb, HHb, COHb, MetHb, sO2, tBili***
Blood Gas, Electrolytes, Glu, Lac, Hct, tHb, O2Hb, HHb, COHb, MetHb, sO2, tBili***
** 31-day onboard use-life, except 600-test PAK which has 21-days.
*** PAKs available with or without tBili.
ꭞ sO2 = O2Hb/O2Hb+HHb
- Lippi G, von Meyer A, Cadamuro J, Simundic A-M. Blood sample quality. Diagnosis. 2018;6(1):25–31. doi:10.1515/dx-2018-0018.
- Lippi G, Salvagno GL, Favaloro EJ, Guidi GC. Survey on the prevalence of hemolytic specimens in an academic hospital according to collection facility: opportunities for quality improvement. Clin Chem Lab Med. 2009;47(5):616–618. doi:10.1515/CCLM.2009.132.
- O’Hara M, Wheatley EG, Kazmierczak SC. The impact of undetected in vitro hemolysis or sample contamination on patient care and outcomes in point-of-care testing: a retrospective study. J Appl Lab Med. 2020;5(2):332-341. doi:10.1093/jalm/jfz020.
- Tóth J, Oláh AV, Petercsák T, Kovács T, Kappelmayer J. Detection of haemolysis, a frequent preanalytical problem in the serum of newborns and adults. eJIFCC. 2020Mar;31(1):6-14. PMID: 32256284; PMCID: PMC7109500.
- Phelan MP, Ramos C, Walker LE, et al. The hidden cost of hemolyzed blood samples in the emergency department. J Appl Lab Med. 2021;6(6):1607–1610. doi:10.1093/jalm/jfab035.
- Phelan MP, Hustey FM, Good DM, Reineks EZ. Seeing red: blood sample hemolysis is associated with prolonged emergency department throughput. J Appl Lab Med. 2020;5(4):732–737. doi:10.1093/jalm/jfaa073.
- Wilson M, Adelman S, Maitre JB, et al. Accuracy of hemolyzed potassium levels in the emergency department. West J Emerg Med. 2020;21(6):272–275. doi:10.5811/westjem.2020.8.46812.
- Milutinović D, Andrijević I, Ličina M, Andrijević L. Confidence level in venipuncture and knowledge on causes of in vitro hemolysis among healthcare professionals. Biochem Med. 2015;25(3):401–409. doi:10.11613/BM.2015.040.
- Nichols JH, Apple FS. Prevalence of hemolyzed results in acute care settings. J Appl Lab Med. 2023;8:431-434. doi:10.1093/jalm/jfac141
- Khedr S, Blake V, Erdogan E. Neonatal unit hemolysis rates from an academic medical center: A quality improvement project. Arch Path Lab. 2016;140(6):502-503. doi:10.5858/arpa.2015-0252-le
- Werfen. GEM Premier 7000 with iQM3 Operators Manual. P/N 00000026407. Rev 00. Aug 2023.
- Dietzen DJ, Jackups R, Zaydman MA. Clinical implications of inaccurate potassium determination in hemolyzed pediatric blood specimens. Clin Chim Acta. 2024;15(557):117862. doi:10.1016/j.cca.2024.117862.
- Wu AHB, Peacock WF. Potential medical impact of unrecognized in vitro hypokalemia due to hemolysis: a case series. Clin Chem Lab Med. 2024;aop:1–5. https://doi.org/10.1515/cclm-2024-0351.
- 17. Azman WNW, Omar J, Koon TS, Ismai TST. Hemolyzed specimens: major challenge for identifying and rejecting specimens in clinical laboratories. Oman Med J. 2019;34(2):94–98.
- 18. Möckel M, Luppa PB. Why hemolysis detection should be an integral part of any near-patient blood gas analysis. J Lab Med. 2021;45(4-5):193–195. https://doi.org/10.1515/labmed-2021-0076.
- Nigro M, Valli G, Marchionne ML, et al. Is there a risk of misinterpretation of potassium concentration from undetectable hemolysis using a POCT blood gas analyzer in the emergency department? Medicina. 2023;59(66):1–11. https://doi.org/10.3390/medicina59010066.
Not available in all countries.
Contact us directly using the below, or by filling out the form.
sales.uk@werfen.com
Tel: 01925 810 141 - Option 6
orders.uk@werfen.com
Tel: 0800 102 6342
service.uk@werfen.com
Tel: 01925 810 141 - Option 1




A breakthrough in blood gas testing: haemolysis detection
In a transformative step toward enhancing patient outcomes in acute care, GEM Premier 7000 with iQM3 provides lab-quality detection of haemolysis, in whole blood.
Informs and expedites critical decision-making3,6,12–16
Now with haemolysis detection, iQM3 ensures sample quality across the most common preanalytical errors (e.g., haemolysis, clots, bubbles). GEM Premier 7000 detects haemolysis in 45 seconds11 helping inform appropriate patient management decisions.
How is whole blood haemolysis detection possible?
GEM Premier 7000 with iQM3 utilises patented technology for haemolysis detection. Based on a photometric measurement of whole blood, the haemolysis module includes: